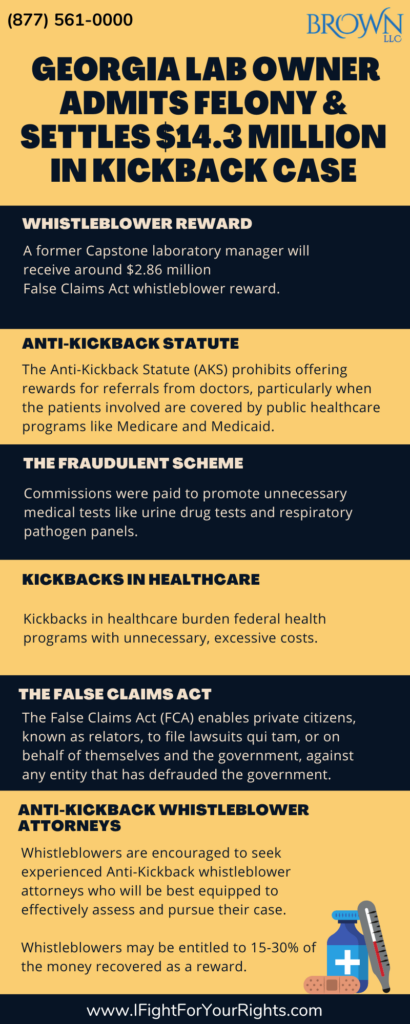
Georgia Lab Owner Admits Felony and Settles $14.3 Million in Kickback Case
Andrew “Drew” Maloney, a 57-year-old owner of the clinical Georgia laboratory, Capstone Diagnostics, admitted to a felony conspiracy to pay healthcare kickbacks and agreed to pay over $14 million to settle his case. [1] A former insider will receive around $2.86 million as a whistleblower reward for his contributions in coming forward with information about Capstone’s fraudulent actions. The success of his case, like other whistleblower cases, relied in part on the strength of his information, and the use of an anti-kickback whistleblower attorney who has experience handling False Claims Act litigation.
Anti-Kickback Statute
The Anti-Kickback Statute (AKS) prohibits the use of undue renumeration in exchange for the inducement of referrals from physicians. Specifically, these referrals are prohibited when the patients in question are covered by publicly funded healthcare programs (such as Medicare and Medicaid). [2] Undue renumeration includes receiving anything of value, such as meals, money, or free rent. Principal Deputy Assistant Attorney General, Brian M. Boynton stated, “The law prohibits healthcare providers, including laboratories, from paying kickbacks to third parties to generate business”. (n 1). Boynton stressed that kickback schemes are corrupt practices that severely hurt the integrity of healthcare programs.
What Happened? The Fraudulent Scheme
The Justice Department’s statement (n 1) showed that Capstone, under Maloney’s approval, targeted vulnerable federal healthcare programs and Georgia Medicaid. Commissions were paid to push for unnecessary medical tests such as urine drug tests and respiratory pathogen panels. Maloney illegally paid portions of Medicaid reimbursements to the operators of an after-school program for urine specimen drug testing samples submitted. Capstone submitted $1 million worth of claims related to the fraudulent drug testing and Georgia Medicaid covered at least $400,000 of the fraudulent claims. Maloney’s sentencing is currently scheduled to take place on May 29, 2024. On top of Maloney’s guilty plea, four other individuals pleaded guilty to their part in the fraudulent drug testing scheme.
Covid-19 Fraud
During 2020 and 2021, Maloney’s laboratory took advantage of the urgency and demand of the COVID-19 pandemic presented. The laboratory forged signatures to order tests and pay unlawful commissions on these tests. Maloney also manipulated the demand for respiratory tests in senior communities to make profits at the expense of federal and state health programs. This demonstrated Covid-19 fraud was extremely common given the extensive funds made available during the pandemic. There are estimated to be billions of dollars still to be recovered from misappropriated pandemic related funds, such as PPP loan fraud.
The Department of Justice showed its commitment to combat COVID fraud with the establishment of the COVID-19 Fraud Enforcement Task Force on May 17, 2021. The DOJ partners with other federal government agencies to investigate and prosecute criminal and civil fraud against relief programs by uncovering fraudulent actors and schemes. [3] The DOJ is especially interested in whistleblowers and their counsel who provide them with insightful and actionable information, and who may be eligible for a whistleblower reward if the case is commenced properly under the False Claims Act and succeeds.
Speak with the Lawyers at Brown, LLC Today!
Over 100 million in judgments and settlements trials in state and federal courts. We fight for maximum damage and results.
Kickbacks in Healthcare
Deceitful practices like kickbacks in healthcare burden federal health programs with unnecessary, excessive costs. Healthcare providers submitting Medicare and Medicaid claims for medically unnecessary services creates a substantial risk of harm to these programs and the patients who rely on them. According to U.S. Attorney Ryan K. Buchanan, “Unfortunately, Capstone and Maloney are hardly alone, as we have witnessed some clinical laboratories and their owners across the country engage in unscrupulous kickback and billing schemes that caused incalculable harm to Medicare”. (n 1). Buchanan followed by emphasizing the office’s commitment to hold people accountable when they steal from federal healthcare programs.
The False Claims Act
The False Claims Act (FCA) was originally passed during the civil war to combat defense contractor fraud. Since then, it has enabled private citizens, known as relators, to file lawsuits qui tam, or on behalf of themselves and the government, against any entity that has defrauded the government. In exchange, these relators are entitled to up to a third of the recovery, if the government does not intervene, and up to a quarter if the government does intervene. So, if a relator recovered $100 million in a lawsuit on behalf of the government, a relator may be entitled up to $30 million of the recovery as a whistleblower award. Since billing done downstream of a kickback is illegitimate, all public billing costs thereafter may be considered FCA violations as well. For example, if a nursing home had 100 patients, all of whom were covered under Medicare, and all of whom were referred by a physician receiving kickbacks, all billing completed by that nursing home may be actionable under the FCA.
Anti-Kickback Whistleblower Attorneys
Employees and other members of the public are urged to keep a keen eye out for fraud and report suspicion of fraud to prevent deceitful schemes like this from persisting. Whistleblowing is one of the most powerful tools to thwart healthcare fraud. Whistleblowers are encouraged to seek experienced anti-kickback whistleblower attorneys, who will be best equipped to effectively assess the strengths of a whistleblower’s claim, and forcefully pursue them. They are the best tool a whistleblower has in maximizing their chance of a successful case and award.