Top 10 Ways to Select the Best False Claims Act Lawyer for Your Case
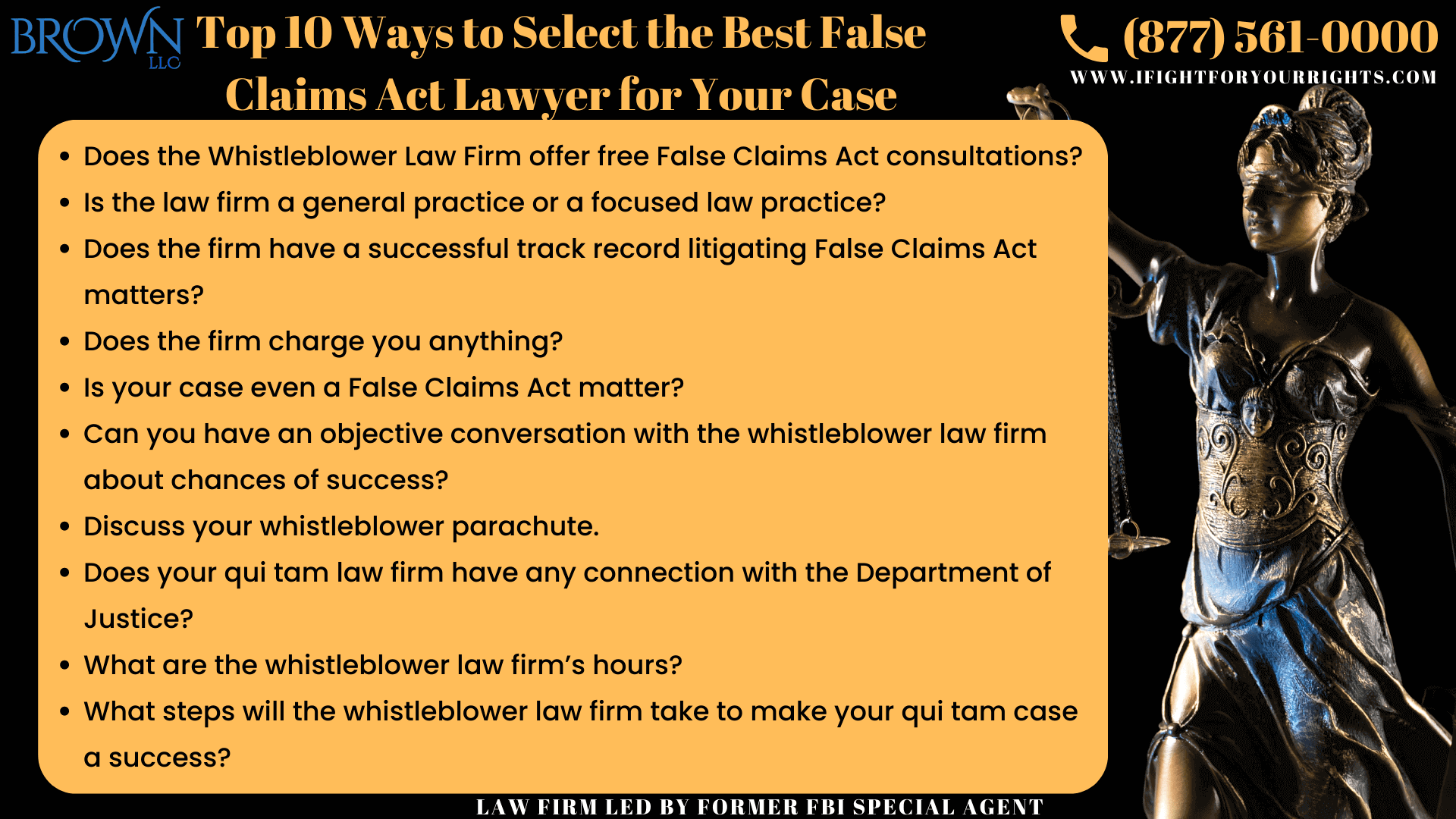
Table of Contents
Many employees work in a field in which billing the federal government is a regular part of the job and by simply paying attention, you may notice that your company’s billing practices often result in overbilling the government, so if that sounds like you and you wish to become a whistleblower, you will need to vet and select the best False Claims Act lawyer for your case. Over the last decade, trillions of aggregate taxpayers dollars have been stolen from government programs with schemes like Medicare Fraud using a Medicare fraud whistleblower lawyer, Medicaid Fraud, Pharmaceutical Fraud, and Defense Contractor Fraud to name a few, which in turn has resulted in billions upon billions in aggregate whistleblower rewards. Sprinkle on top the record spending of the federal government and the cash lifelines that were handed out during the pandemic then you can also look at PPP Loan Fraud, customs fraud, not to mention other programs such as anti-money laundering whistleblower programs (AML), SEC whistleblower programs using an SEC whistleblower attorney, CFTC whistleblower programs, and NHTSA whistleblower programs, all of which will be topics for another day. Objectively based on the number of cases filed, the whistleblower law firm of Brown, LLC has been constantly at the top of volume and performance over the last half-decade or so, based on the independent analysis of Lex Machina and its whistleblower awards and results. Here are some insights from their storied whistleblower law firm about the top 10 ways to select the best False Claims Act lawyer for your case:
Does the Whistleblower Law Firm offer free False Claims Act consultations?
Certain firms charge for their legal consultations. The False Claims Act is constantly evolving in its application and the way the courts enforce it and what is needed to even file a case in court. Certain firms will charge you for a False Claims Act consultation leveraging their experience to command a certain price, while other whistleblower law firms may charge you to research a discrete issue. On the False Claims Act defense side it is much more common to charge, but for the best false claims act lawyers on the plaintiffs side, they will generally offer free whistleblower consultations like Brown, LLC does.
Is the law firm a general practice or a focused law practice?
The world of false claims act litigation is not for the outsider – by its very nature the False Claims Act statute relies on insiders to serve as whistleblowers and similarly the system prefers the firms that have experience in whistleblower litigation. In fact, under the False Claims Act, it is prohibited to bring a matter pro se – that means, you can’t file a case without a whistleblower law firm – one of the few areas of law where an individual can’t proceed on their own. This is analogous to a corporate entity which generally requires a lawyer to represent it in court. It is slightly different, because a qui tam case under the False Claims Act the plaintiff is referred to as a relator, since the plaintiff is relating the case of the federal government through their complaint. The federal government does not want bad law created in the False Claims Act arena, so they will invariably pressure firms who do not know what they are doing or who have the potential to create bad law to dismiss their case and sometimes move for dismissal over the firm’s objections. After the case is initially filed confidentially under seal, the government has the first look at it and will often try to discourage the whistleblower from proceeding if the government doesn’t like the case, the whistleblower, or the whistleblower’s attorneys. There’s only a handful of very established qui tam law firms and even a smaller set that have actually proceeded with the false claims act litigation and succeeded after the government has declined the matter. The whistleblower law firm of Brown, LLC is one of the few firms that has in the past and is presently as of this writing litigating cases the government turned down and has a qui tam unit dedicated to protecting the whistleblower.
Does the firm have a successful track record litigating False Claims Act matters?
Although there’s a common disclaimer in the legal world that past results don’t guarantee future success, past results are certainly indicative of accomplishment. Brown, LLC consistently grades up at the top of the list as one of the best whistleblower law firms when examining their track record of litigation.
Speak with the Lawyers at Brown, LLC Today!
Over 100 million in judgments and settlements trials in state and federal courts. We fight for maximum damage and results.
Does the firm charge you anything to take your whistleblower case?
The best whistleblower law firms generally take qui tam litigation under the False Claims Act on a contingency basis, meaning they’re only paid if they win your case. So essentially, they’re working for free unless they obtain a result. Brown, LLC primarily takes whistleblower matters on a fully contingent basis and under the False Claims Act exclusively litigates on a contingency basis.
Is your case even a False Claims Act matter?
The world of whistleblower law enjoys a broad spectrum of statutes to navigate through and invoke. A False Claims Act case is a very particularized type of case involving the defrauding of the federal government or the state government or involving kickbacks or self-dealing (e.g., a Stark Act violation). Speaking with an experienced whistleblower law firm can assist in evaluating your eligibility to file a False Claims Act lawsuit or potentially other types of whistleblower cases.
Can you have an objective conversation with the whistleblower law firm about chances of success?
In the secret world of whistleblowers under the False Claims Act, you don’t know what you don’t know, and what you do know you better put in front of the government efficiently because there is a first to file rule that may preclude subsequent filers from any recovery. That’s just one factor that goes into the potential for success, but others include the amount of government funds implicated, the strength of the proofs, whether an individual specimen of the fraud exists from start to finish, the law in the jurisdiction you’re filing the qui tam claim to name a few others. An experienced false claims act law firm can help give you some handicapping regarding chances of success, but nothing is ever guaranteed. However, if the firm takes the whistleblower case on contingency and is willing to work on a matter with the risk it’ll never be paid, that can indicate the degree of the firm’s belief in you and your whistleblower case.
Discuss your whistleblower parachute.
Some of the best whistleblower law firms will discuss the lawsuit not just in terms of the glacial pace that most qui tam lawsuits seem to take, but also to provide well rounded context and a plan for you as a whistleblower about what your exit strategy is for the company. Although the various whistleblower statutes, including the False Claims Act, provide strident protections against retaliating against a whistleblower, there’s always a chance the company will do something in retaliation. As a litigant under the False Claims Act you have the benefit of time to plan for your exit if you want to leave your company as the case is initially filed confidentially under seal. Also, if the company is engaging in conduct that is illegal, unethical, reprehensible or a blend of the three, you have to ask yourself is that an entity you wish to stay with as your career reputation may be impacted. Quality qui tam law firms who have navigated the landmines of the litigation in the past will best help you plan for the future.
Does your qui tam law firm have any connection with the Department of Justice?
The Department of Justice (DOJ) is an entity onto itself shrouded in secrecy at times and has its own behaviors and rules that must be respected even if you personally or politically disagree with the perception of them. They are the ones that have the ultimate say about intervening in the case or if they decline, allowing you to litigate the false claims act declination. Furthermore, if you are litigating a declined false claims act case, they will have to sign off on any settlement. You can’t go into the whistleblower litigation as an ambassador for the government as a relator with the mindset that the government is the enemy, because ultimately, they will hold the keys to your fate in the qui tam world. The best whistleblower law firms often have former officials from the Department of Justice to help seamlessly interface with what is sometimes a very labyrinthine process. The head of the firm Brown, LLC and the co-chair of the whistleblower department worked for the Department of Justice and was a former Special Agent and Legal Advisor for the Federal Bureau of Investigation (FBI).
What are the whistleblower law firm’s hours?
As a potential whistleblower you may need to speak after hours or during the weekend when it’s more convenient for you and not when you are in the confines of the work environment where and when the fraud is occurring. Brown, LLC handles cases nationwide, has whistleblower lawyers deployed from east to west coast and will make arrangements to speak at your convenience.
What steps will the whistleblower law firm take to make your qui tam case a success?
Every case has its own personality and firms like Brown, LLC who are incentivized to make your qui tam case a success by aligning its economics with the success of your case by taking the case on contingency. The whistleblower team at Brown, LLC functions as a team which is critical. Defendants are plotting to commit the fraud, and it takes a team effort to try and unearth it. Firms like Brown, LLC are constantly working the case even if it seems quiet, monitoring the file, interfacing with the DOJ, and looking for ways to push the case forward with the DOJ or to settlement or trial if it’s a declined qui tam matter.
There’s a lot in play if you’re thinking about blowing the whistle and one of the first things you should do is look for the best False Claims Act lawyer for your matter. The best law firms make time for their clients, align their economic interests with the client’s and work hard to make the case a success. When canvassing for a qui tam firm, you should consider Brown, LLC as one of the best whistleblower law firms available and take advantage of their offer to provide you with a free whistleblower consultation.
Working With a False Claims Act Attorney
To file claims under the False Claims Act, it is required to use a whistleblower law firm as an individual cannot file the matter pro se (without an attorney) since the lawsuit seeks to represent the United States’ interests as well as the relator’s (a qui tam term for whistleblower). One should consult a False Claims Act attorney regarding the circumstances of the case to determine whether to file it, and make sure it’s presented in the best possible manner. A False Claims Act lawyer can aid in structuring a case, lawfully compiling documents, and most importantly, the whistleblower could have the benefit of the firm’s experience to navigate them through any issues that may arise.
If you’re looking to take the next step, here are the top 10 ways to select the best False Claims Act lawyer for your case to help you make an informed choice in legal representation.
Experienced False Claims Act attorneys also ensure that the facts of a whistleblower’s case are succinctly and persuasively presented, giving such reports a competitive edge over those submitted by a general practitioner. Since cases under the FCA are filed and presented to the Department of Justice, it is helpful to look for a firm who has a track record of success in this space and further, that has former DOJ individuals, like FBI agents or FBI Legal Advisors.
Qui tam cases are filed under seal, meaning the complaint does not initially appear on the public docket and the investigation proceeds without notifying the defendant. This is done in the interest of the government’s investigation so it can proceed without complications. This also ensures that the whistleblower’s identity remains confidential until the seal is lifted or partially lifted at the conclusion of a case. The False Claims Act also prohibits retaliation against employees acting in the capacity of a whistleblower.
While there may be fraud that accompanies all economic growth, there are sophisticated legal mechanisms in place to combat fraud and recover illegally obtained funds. Whistleblowers continue to be the pivotal components to fraud recovery efforts, since it is through their intervention that the proper authorities can respond to and deter fraud.
Check out this analysis on how False Claims Act settlements and judgments surpassed $2.68 billion in fiscal year 2023.
