How to Choose the Best Whistleblower Attorneys in Medicare Fraud Cases

Table of Contents
Medicare fraud is a serious issue that not only costs the government billions of dollars but also adversely affects the lives of countless individuals who rely on this essential healthcare program. Thankfully, there are laws and incentives in place to encourage individuals with knowledge of Medicare fraud to come forward as whistleblowers by properly invoking the False Claims Act. These brave individuals, often employees or insiders with valuable information, can make a substantial impact by exposing fraud within the healthcare system. To navigate the complex process of reporting and litigating Medicare fraud, you need to find the best whistleblower attorneys and the best whistleblower lawyer for your case.
In this blog post, we will explore the critical role of whistleblower attorneys, discuss the False Claims Act Medicare fraud whistleblower reward program, and provide insights into how to select the right qui tam law firm for your case. Whether you are a pharmaceutical whistleblower or have knowledge of Medicare fraud in any other capacity, this guide will help you make an informed decision when choosing the best whistleblower attorney.
The Crucial Role of Whistleblower Attorneys
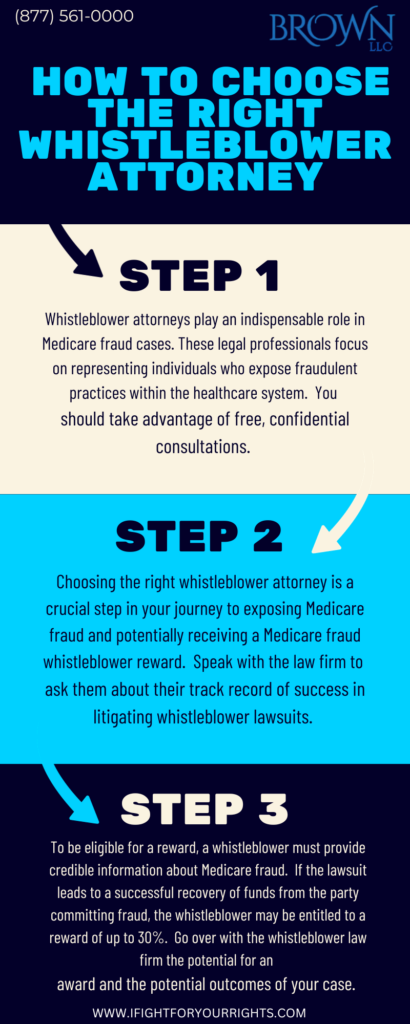
Whistleblower attorneys play an indispensable role in Medicare fraud cases. These legal professionals focus on representing individuals who expose fraudulent practices within the healthcare system. Here’s why their role is so vital:
- Experience in Healthcare Fraud Laws: The best whistleblower attorneys are well-versed in the complex web of federal and state laws that pertain to healthcare fraud, including the False Claims Act. They understand the nuances of these laws, which is crucial for building a successful case.
- Guidance Through the Legal Process: Whistleblowing can be a daunting process, with significant legal and personal implications. An experienced attorney can provide guidance and support at every stage, ensuring you understand your rights and responsibilities.
- Protection Against Retaliation: Whistleblowers often face the risk of retaliation from their employers. A whistleblower attorney can help shield you from these adverse actions, ensuring your rights are upheld.
- Maximizing Whistleblower Rewards: When a whistleblower’s case leads to a successful prosecution, they may be entitled to a Medicare fraud whistleblower reward. Whistleblower attorneys have the experience to negotiate the highest possible reward for their clients.
Understanding the Medicare Fraud Whistleblower Reward Program
One of the most significant incentives for whistleblowers to come forward with information about Medicare fraud or Medicaid fraud is the potential for financial rewards. The Medicare Fraud Whistleblower Reward Program, established under the False Claims Act, offers whistleblowers the opportunity to receive a portion of
the recovered funds. This can be a substantial sum, making it a compelling reason to blow the whistle on fraud.
Here’s how the Medicare fraud whistleblower reward program works:
- Reporting the Fraud: To be eligible for a reward, a whistleblower must provide credible information about Medicare fraud. This typically involves submitting a qui tam lawsuit using a whistleblower law firm, which is a legal action filed on behalf of the government.
- Government Investigation: Once a qui tam lawsuit is filed, the government will investigate the claims. If the government decides to pursue the case, it may join the whistleblower’s lawsuit.
- Recovery and Reward: If the lawsuit leads to a successful recovery of funds from the party committing fraud, the whistleblower may be entitled to a reward. The reward typically ranges from 15% to 30% of the total amount recovered.
- Protection from Retaliation: Whistleblowers are also protected from retaliation by the False Claims Act, which prohibits employers from taking adverse actions against employees who report fraud.
Speak with the Lawyers at Brown, LLC Today!
Over 100 million in judgments and settlements trials in state and federal courts. We fight for maximum damage and results.
Choosing the Best Whistleblower Attorney
Selecting the right whistleblower attorney is a critical decision that can significantly impact the success of your case and the potential reward you may receive. To make an informed choice, consider the following factors:
- Experience and Skill: Look for an attorney with a track record of handling whistleblower cases, particularly those related to Medicare fraud. Their experience can be invaluable in navigating the complexities of these cases.
- Resources: Investigating and litigating healthcare fraud cases can be expensive and time-consuming. Ensure that the attorney and their law firm have the resources necessary to handle your case effectively.
- Understanding of Healthcare Laws: Medicare fraud cases are governed by a unique set of laws and regulations. Your attorney should have a deep understanding of healthcare laws, including the False Claims Act and Anti-Kickback Statute.
- Success Record: Inquire about the attorney’s success rate in achieving favorable outcomes for their clients. A proven track record demonstrates their ability to handle whistleblower cases effectively, but past results don’t guarantee future success.
- Communication and Trust: Building a strong attorney-client relationship is essential. You should feel comfortable discussing your case with your attorney and trust their advice and guidance.
- Reputation and Reviews: Research the attorney’s reputation in the legal community and read reviews from past clients to get a sense of their capabilities and professionalism.
- Fee Structure: Understand the attorney’s fee structure and whether they work on a contingency basis. Most whistleblower attorneys work on a contingency fee, meaning they only get paid if you win your case.
Choosing the right pharmaceutical fraud lawyer is a crucial step in your journey to exposing Medicare fraud and potentially receive a substantial Medicare fraud whistleblower reward. Whistleblower attorneys possess the skill, resources, and experience necessary to navigate the complex legal landscape surrounding healthcare fraud.
If you are a pharmaceutical whistleblower or have knowledge of Medicare fraud in any capacity, don’t hesitate to seek the legal representation you need. By selecting the best whistleblower attorney, you can help protect the integrity of the Medicare system, hold fraudsters accountable, and potentially benefit from the Medicare fraud whistleblower reward program. Your actions could make a significant difference in the fight against healthcare fraud.