Medicare Whistleblowers: FAQ
Medicare fraud is a major problem that costs taxpayers billions of dollars and can harm patients by providing unnecessary or low-quality care. It can take many forms and be perpetrated by anyone involved in the healthcare system, including doctors, nurses, hospitals, and even by pharmaceutical companies.
Recognizing the signs of Medicare fraud is critical in order to help prevent it. As a Medicare whistleblower, you have the ability to aid in the prevention of fraud and the integrity of the Medicare program and further, if you blow the whistle the right way you can potentially receive a whistleblower award of up to 30% of what the government recovers. With an estimated tens of billions of dollars a year of Medicare fraud, that’s hundreds of millions of dollars available to whistleblowers for doing the right thing.
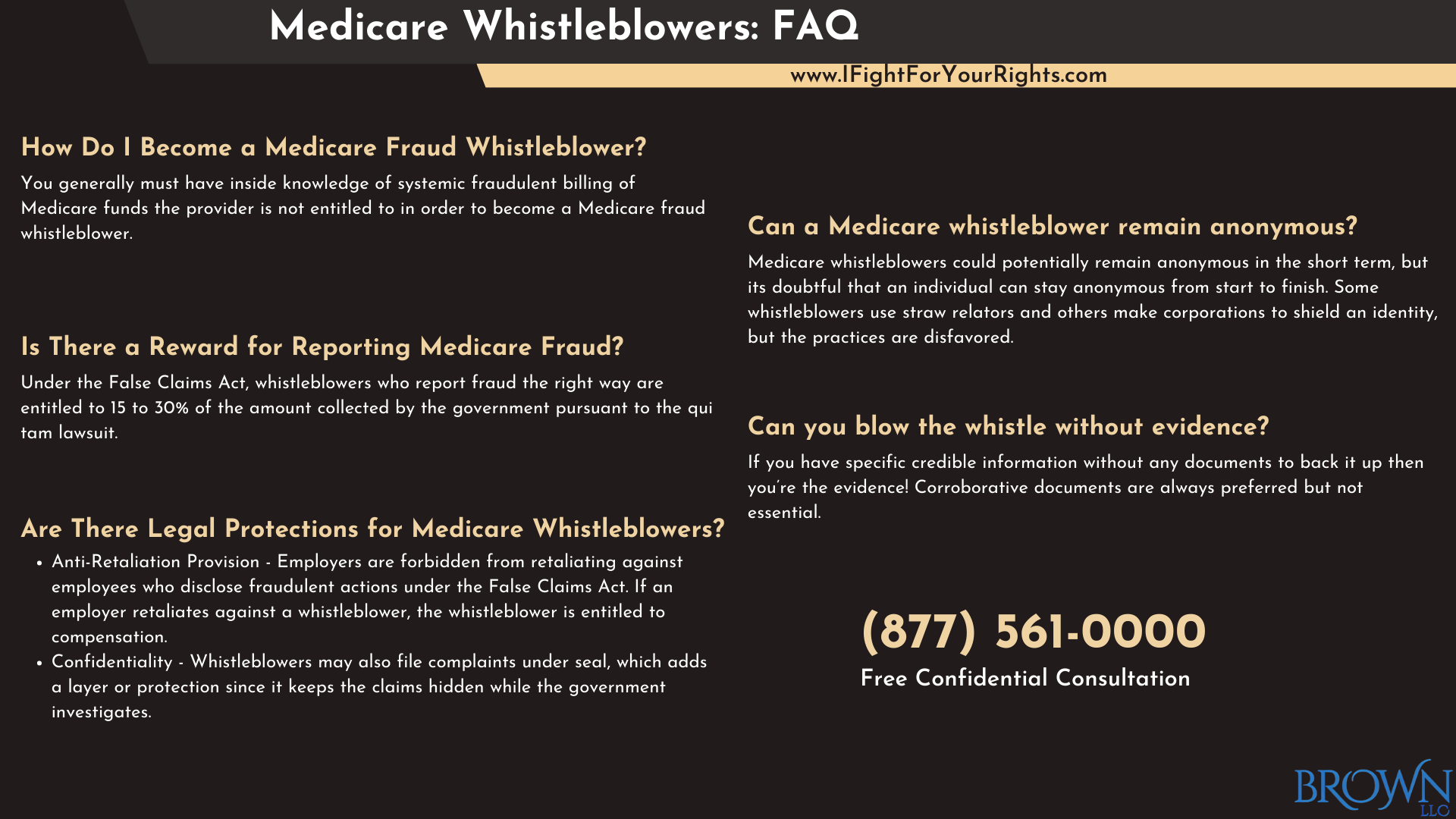
How Do I Become a Medicare Fraud Whistleblower?
You generally must have inside knowledge of billing and the receipt of Medicare funds that were either not rightfully earned and/or not performed, and/or overinflated to become a Medicare fraud whistleblower. A Medicare fraud lawyer will then file a legal claim under a program that specifically targets the type of fraud you’ve unearthed by utilizing the False Claims Act (FCA). There are other whistleblower programs that you can also file under, but only if the fraud extends to other purviews, but sometimes, where there’s smoke there’s fire. The other whistleblower programs include, but are not limited to, the Securities and Exchange Commission (SEC) Whistleblower Program if it implicates a publicly traded company, and the Internal Revenue Service (IRS) Whistleblower Program if taxes are falsified and/or obscured.
Each whistleblower program has its own set of rules on how to file, how long you have to file, and your whistleblower rights. You should consult with a Medicare whistleblower lawyer who will help properly prepare your claim and maximize your chance to receive a potential whistleblower reward.
Speak with the Lawyers at Brown, LLC Today!
Over 100 million in judgments and settlements trials in state and federal courts. We fight for maximum damage and results.
Is There a Reward for Reporting Medicare Fraud?
Under the False Claims Act, whistleblowers who report instances of Medicare or Medicaid fraud are financially rewarded, with rewards ranging from 15 to 30% of the amount collected by the government based on their report.
To be eligible for a False Claims Act award, the whistleblower must hire a Medicare whistleblower lawyer and file an action confidentially under seal against the healthcare provider or hospital or pharmaceutical company involved in the fraudulent activities.
How Does Whistleblower Law Prevent Medicare Fraud and Abuse?
Whistleblower laws are important in preventing Medicare fraud and abuse because they encourage people with insider information to come forward and report such activities. These laws protect and compensate whistleblowers who expose fraudulent or abusive Medicare or Medicaid practices by healthcare providers.
Whistleblower laws protect against Medicare fraud and abuse by encouraging people to come forward with information, allowing the government to take legal action against perpetrators, and discouraging healthcare providers from engaging in fraudulent activities in the first place.
Are There Legal Protections for Medicare Whistleblowers?
Yes, whistleblowers under Medicare are legally protected. The False Claims Act, the primary law used to combat healthcare fraud, contains protections that shield whistleblowers against retaliation by employers for reporting fraud. Among the Medicare whistleblower protections are the following:
Anti-Retaliation Provision: Employers are forbidden from retaliating against employees who disclose fraudulent actions under the False Claims Act. If an employer retaliates against a whistleblower, the whistleblower is entitled to retaliation compensation, which includes double back pay, reinstatement, and reimbursement for any particular damages suffered as a result of the retaliation, as well as attorney’s fees and costs.
Confidentiality: Whistleblowers may also file complaints under seal, which keeps the claims hidden while the government investigates. This rule protects whistleblowers from initially being recognized and punished by their employers.
Whistleblowers who report Medicare fraud and abuse the correct way are protected by a variety of federal laws that offer legal protections, confidentiality, monetary rewards, and other safeguards to encourage and protect those who report fraudulent activities.
Is There a Deadline to File a Medicare Fraud Lawsuit?
Yes, there is a time limit for filing a lawsuit alleging Medicare fraud. The statute of limitations under the False Claims Act is six years from the date of the fraud or three years from the date the government knew or should have known about the fraud, whichever comes first. However, that statute may shrink or enlarge depending on certain circumstances. You can’t rely on this to determine your statute of limitations. For any statute of limitations questions you must retain a whistleblower attorney to give you a legal opinion on the situation.
Can a Medicare whistleblower remain anonymous?
Medicare whistleblowers could potentially remain anonymous in the short term, but it’s doubtful in the long term. Under the False Claims Act, whistleblowers can file lawsuits under seal, which means the lawsuit is kept private while the government investigates the allegations. Sometimes people try to file False Claims Act lawsuits using a corporation or a straw realtor, but overall neither technique is recommended as it creates additional layers of complications.
When compared to other whistleblower laws, maintaining anonymity as a whistleblower in cases reported to the SEC or CFTC may be easier. The SEC, CFTC, NHTSA and AMLA statutes have provisions that allow an individual to anonymously report violations through the use of an attorney, and while there’s a good chance in those programs you can stay anonymous from start to finish, there’s still a chance that your identity is disclosed.
Can you blow the whistle without evidence?
The word evidence is very broad. If you have very specific credible information without any documents to back it up then you’re the evidence! Corroborative documents are always preferred but not essential. Blowing the whistle can be difficult without corroboration, and authorities may take no action depending on how you present yourself as a realtor. A relator is a term for a plaintiff under the False Claims Act since the individual is relating the case to the government through their own complaint. Whistleblowers are typically expected to provide specific, credible information or evidence to support their claims. It may be difficult to persuade authorities to launch an investigation or take legal action in the absence of corroborative evidence.
It is still possible to report suspicions of wrongdoing or misconduct without concrete evidence, but it is critical to consult with a Medicare fraud attorney to learn about your rights about how to do so. Suspicions in a vacuum alone won’t suffice, but if you have a free, confidential whistleblower consultation with a firm then perhaps they can help elicit information that’s more concrete that goes beyond just mere suspicions. Please note, it’s never a good idea to conduct an investigation by yourself without guidance, and if you were to do so you should never access information you’re not entitled to see or you may land yourself into trouble.
Whistleblowers in Medicare play an important role in preventing Medicare fraud and abuse. If you have knowledge of fraudulent Medicare activities, speak with a Medicare whistleblower lawyer to learn more about your rights and options. Remember that whistleblowers are legally protected, and you could receive a financial reward for your information if presented in the right manner.
