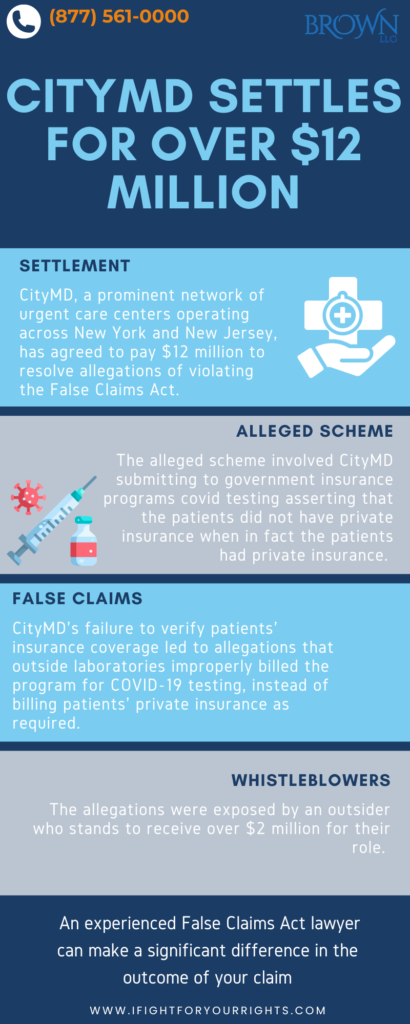
CityMD Settles for Over $12M for Alleged False COVID-19 Claims
Table of Contents
CityMD, a prominent network of urgent care centers operating across New York and New Jersey, has agreed to pay $12.04 million to resolve allegations of violating the False Claims Act. This settlement demonstrates the government’s continued prioritization of using the False Claims Act to tackle COVID-19 healthcare fraud. The alleged scheme involved CityMD submitting to government insurance programs COVID testing asserting that the patients did not have private insurance when, in fact, the patients had private insurance. So, they were allegedly making the taxpayers pay for testing covered by their private insurance, a direct violation of the billing guidelines. The False Claims Act whistleblower, for his efforts, will receive over $2 million as a whistleblower reward. The whistleblower was just an attentive patient who experienced the scheme and was shrewd enough to have an experienced False Claims Act law firm file a well-pled qui tam complaint – which underscores that even outsiders can blow the whistle on a fraud if they bring it to the attention of the government in the right way.
COVID-19 Reimbursement Program for Testing, Treatment, and Vaccine Administration for the Uninsured
During the COVID-19 Pandemic, the Health Resources & Services Administration (HRSA) program created a program for reimbursing providers. As long as the provider did its due diligence to determine whether or not the tested patient already had their own insurance, the program allowed for healthcare providers and facilities to submit for reimbursement for COVID-19 testing, treatment, and vaccinations for uninsured individuals. In return, the provider would benefit by receiving compensation at Medicare rates for these uninsured individuals.
Accusations of CityMD’s Improper Billing Practices During COVID-19
However, CityMD was accused of improperly abusing this program. For almost two years, the network was alleged to knowingly submit false claims requesting payment with no regard as to whether the patients tested had their own health insurance coverage, which in those instances dictated submitted it to the private insurance instead of the taxpayers. The Department of Justice (DOJ) pointed to the foundation for the fraud was CityMD submitting claims for patients without determining if they were actually insured by their own private insurance and then submitting the claims to the government even though they had private insurance, which was expressly and logically prohibited. CityMD was even alleged to have taken patient’s private health insurance cards which were included in their patient files which means they were acutely aware that the individual had their own private insurance and that the claim should not have been submitted to the government. Because of CityMD’s lack of proper verification to see if patients had coverage, and at times willful indifference to the knowledge that they had private insurance, outside laboratories were alleged to have submitted false claims for COVID-19 testing to the program when private insurance should have been billed instead.
Speak with the Lawyers at Brown, LLC Today!
Over 100 million in judgments and settlements trials in state and federal courts. We fight for maximum damage and results.
The Role of Whistleblowers in the Claims Against CityMD
Whistleblowers are often insiders who have information to allege the details of the scheme, but occasionally an outsider can succeed with their False Claims Act complaint with a skillfully drafted complaint and some detailed skeleton for the scheme along with a specimen. These accusations against CityMD were brought to light through the efforts of a whistleblower, a patient at CityMD, who filed a qui tam lawsuit under the False Claims Act. The False Claims Act allows for private parties to file an action on behalf of the United States for alleged fraud against the government with the use of a whistleblower law firm. Of the $12 million settlement that the government secured against CityMD, Kitzinger was entitled to receive $2,046,308 for his efforts as a whistleblower award.
Whistleblowers are entitled to a percentage of the recovered funds in a successful False Claims Act case. If the government intervenes, whistleblowers can receive between 15% and 25% of the total recovery. If the government does not intervene and the whistleblower proceeds with the case, they may receive between 25% and 30% of the recovery. For the whistleblower, he received close to 17%, which resulted in a takeaway of $2 million whistleblower reward. Imagine going into the clinic with a runny nose and coming out with a $2 million award for doing the right thing.
How a Finto Claims Act Whistleblower Lawyer Can Assist in a COVID-19 Fraud Claim
In cases of healthcare fraud related to COVID-19, such as the CityMD case, a False Claims Act law firm can play a critical role in assisting whistleblowers meet the evidence threshold for a viable claim, especially if someone is on the outside or even on the inside and is looking for guidance about the framework of putting together the case. False Claims Act lawyers will assist by effectively presenting to government investigators all relevant documentation and testimony in a manner they’re used to receiving. This meticulous presentation enhances the chances of the government intervening, which can lead to higher financial recoveries for the whistleblower. Even though the percentages are lower when the government intervenes, the settlement amounts on average are higher. An experienced whistleblower lawyer can make a significant difference to the outcome of your claim, since it is a very particularized field.
For more insights on how healthcare fraud impacts the system and how you can report it, see: Healthcare Fraud: How It’s Harming the System & How You Can Report It.
The government is dedicating substantial resources to combat COVID fraud. Thousands of people have been prosecuted for overbilling the government, wrongfully billing the government, improper and illegal use of loan monies, PPP loan fraud. There are still billions that the government has yet to tackle, so using a 20% relator share as a benchmark, that’s hundreds of millions of whistleblower awards still out there if you blow the whistle the right way.
The False Claims Act also provides protections against retaliation for whistleblowers. Employees who face discrimination or retaliation for their involvement in false claim actions are entitled to remedies, including reinstatement, back pay, and other compensatory damages. A False Claims Act law firm will make sure that you are fully protected to the extent possible under the law.
CityMD’s False Claims Act settlement of over $12 million for submitting false claims to the COVID-19 Uninsured Program highlights the government’s dedication to combating healthcare fraud. The alleged violations of billing the government for COVID-19 tests for patients who had private insurance, thus misusing taxpayer funds, were squarely remedied through this whistleblower action. Another important stream from this story is that the allegations came to light through an outsider who will receive over $2 million for his role in exposing the fraud. The qui tam settlement also emphasizes the ongoing efforts and prioritization of DOJ resources to ensure proper use of pandemic relief funds.